|
NHS
National
Health Service Trusts
Nurse
suspended 'for speaking out' - 19/
6/2007
A
SENIOR nurse suspended after organising industrial action has accused
health bosses of trying to curb her union activities.
Karen Reissmann, a community psychiatric nurse for 25 years, was
suspended by Manchester Mental Health and Social Care Trust (MMHSCT) for
bringing its reputation into disrepute.

Karen
Reissmann
The trust said it had lost confidence in Ms Reissmann . . . on the day
she received a letter confirming her promotion to senior psychiatric
nurse following a staff review.
Earlier this year, Ms Reissmann, Unison branch representative for MMHSCT,
organised a series of protests by 250 staff against planned cuts,
including two one-day strikes.
Unison has held an emergency meeting and 100 staff voted for a ballot on
strike action over Ms Reissmann's suspension.
Ms Reissmann, 48, from Hulme, said: "What I'm guilty of is
defending the NHS and its services for staff and patients and I cannot
stop doing it. I believe in the NHS, that's why I want to work for it.
"What I'm not guilty of is harming a single patient in the process.
I'm disgusted that in 2007 under a Labour government I'm facing
disciplinary action and suspension for trade union activities and
speaking out."
Ms Reissmann has been told she is facing charges of activities seriously
affecting the reputation of the care trust; behaviour undermining their
confidence in her as an employee; and suspected of misusing her time as
a community psychiatric nurse.
She has been particularly critical of the transfer of NHS services to
the voluntary sector, and is facing legal action over her comments
published in a social enterprise magazine in January.
Banned
She has been banned from having contact with patients and was made to
hand over her mobile phone which they ring in an emergency. When the
M.E.N. rang it no one was answering her calls.
A spokesman for MMHSCT refused to respond to claims they were trying to
clamp down on union work. He said: "We do not comment on individual
cases. Suspension is without prejudice and is not regarded as a
disciplinary measure but as a means of carrying out further inquiries.
Community Mental Health Team service users each have a crisis care plan
which advises them on how to access services in a crisis.
"The trust has ensured an effective handover of service-user care
in this case."
As well as the strike, Unison organised 100 staff to drive through city
centre streets to protest at proposals to cut 33 community nurses and
eight occupational therapists from MMHSCT, while increasing the number
of managers and social workers. Steve Stott, regional officer for
Unison, said: "We vigorously defend our members' rights to speak
out without fear of persecution."
http://www.manchestereveningnews.co.uk/
Amanda Crook
BBC
News Tuesday, 29 March, 2005
Psychiatric staff are being put at risk because of inadequate training
and funding, according to the Royal College of Nursing.
"Patients
are frustrated because they're not getting the care they should and
frustration leads to violent behaviour," spokeswoman Ann Leedham-Smith
told File On 4.
More
than 100,000 violent incidents occur across the NHS each year, almost
half in mental health units.
File
On 4 also investigated relatives' concerns over security at a
psychiatric unit where four patients committed suicide
last year.
'Culture
of failure'
The
Department of Psychiatry at the Royal South Hants Hospital was treating
a 29 year-old man for schizophrenia when he stabbed himself to death
with a knife he had smuggled into the ward. In another case, a severely
depressed woman was able to walk out of the hospital and jump into a
river.
Chief
Executive of the Hampshire Partnership Trust, Martin Barkley, said:
"We thought we had a robust system in place but this was proven not
to be the case by the way that Mary Conduct left the Department of Psychiatry,"
he said.
He
denied claims from the Southampton branch of the charity Mind that there
was "a culture of failure" within the unit. "What
we need to do is improve the therapeutic environment and the
relationships between staff and patients."
'Few
permanent staff'
He
said the trust, which was short of around 30 staff psychiatric nurses
last summer, had spent £500,000 in four years improving the wards. The
Sainsbury Centre for Mental Health said shortfalls in government funding
for mental health were impacting on in-patient psychiatric wards.
Chief
Executive Angela Greatley said: "Mental health has not kept pace
with the rest of funding on the NHS and Social Services. "Some
acute in-patient wards have acquired a bad reputation, others will have
few permanent staff, and therefore the thing can become a spiralling
down of the quality of staff in some difficult units."
In
a statement, the Department of Health said that spending on mental
health in England had gone up by 19% in real terms since 1999. And that
an extra £30 million had been made available for psychiatric intensive
care units last December.
'Aggression
and violence'
File
On 4 investigated another patient death in South Wales which took place
against a background of deficiencies in staffing levels and training.
Kurt
Howard, 32, died while under restraint within a fortnight of being
admitted to the Cefn Coed hospital in Swansea in June 2002.
An
internal inquiry into the death carried out by the Swansea NHS Trust
said that three assistants, who were not qualified nurses, and one
psychiatric nurse had taken part in the restraint.
It
found that "the level of training in the management of aggression
and violence that the staff nurse had undertaken was inadequate to
manage this situation." The
panel was also concerned to discover that it was normal practice to have
one qualified member of nursing staff on the ward, where violent
incidents where common.
Swansea
NHS Trust told File On 4 they had made improvements in medical staff,
care plans and training in restraint techniques. But they made it clear
they had a continuing shortage of psychiatric nurses.
Nurse
assaulted
Other
mental health experts told the programme of recruitment difficulties in
in-patient units across England because of a preference among
psychiatric nurses to work in the newer community mental health teams.
Another
consequence of this, said the Royal College of Nursing, was an increase
in violent attacks on its staff caring for disturbed and aggressive
patients. The
union wants more training for nurses in areas such as restraint
techniques and more of their attackers prosecuted.
One
case they are pursuing concerns a psychiatric nurse who was attacked at
Birmingham's Queen Elizabeth psychiatric hospital just weeks after
qualifying. She
was the second person on a particular ward to be assaulted that day and
had received no training in restraint.
The
mental health trust which runs the hospital said such training was
mandatory, but that some new staff may not receive it for weeks or
months after they had begin work.
The
Department of Health told File On 4 that attacks against NHS staff were
wholly unacceptable and that it was working to develop training for
staff in how to prevent and de-escalate such violence.
http://news.bbc.co.uk/1/hi/programmes/file_on_4/4371957.stm

Patricia
Hewitt - Uphill Struggle
PAID
TO KEEP QUIET SCANDAL
NHS
STAFF BANS 500 doctors and nurses suspended £100m a year cost for the
NHS It's 'just to stop whistleblowers'
HUNDREDS
of doctors and nurses are suspended on full pay in a bid to silence
whistleblowers, campaigners claimed yesterday.
Julie
Fagan, of nurses' group Cause - Campaign Against Unnecessary Suspensions
and Exclusions - said: "People are being excluded on the basis of
unsubstantiated allegations and often within days of them highlighting
an area that could cause embarrassment. "Put
simply, it's the quickest and easiest way to get whistleblowers to shut
up."
It
follows a Daily Mirror investigation that found the NHS is spending
millions paying more than 500 doctors and nurses to stay at home. At
least 375 nurses, 152 doctors and 35 other clinical staff are suspended
on full pay from hospitals and GPs' surgeries. And
campaigners claim many are just to "get whistleblowers to shut
up".
The
suspensions are costing the NHS up to £100million a year - a fifth of
the £500mil-lion it overspent last year. That
could build two new hospitals, pay for 5,000 courses of breast cancer
drug Herceptin or 10,000 heart bypass operations. It could also buy 100
MRI scanners, 130 radiotherapy machines or train 2,000 nurses.
The
figures, uncovered under the Freedom of Information Act, show kidney,
bladder and orthopaedic surgeons are the largest group of consultants
suspended, alongside gynaecologists and anaesthetists.
Yet
while doctors with lifesaving skills are paid to stay home, trusts are
cancelling operations and laying off thousands of staff to balance their
books. In
West Midlands, where more than 2,000 jobs are being axed in five
hospitals, 19 doctors and 45 nurses are suspended on full pay.
Some
suspensions are for valid reasons such as medical malpractice but some
other staff are excluded for apparently flimsy reasons. One senior
consultant was sent home for "not being a team player" and a
radiologist for "an unauthorised audit".
And
increasing numbers of staff claim they are suspended for raising
concerns about poor practice or patient safety. Some
doctors and nurses claim they have been banned from work just because of
personality clashes with their managers.
They
are forced to stay at home while trusts conduct investigations into
alleged offences such as "bullying" or "harassment".
An
average suspension lasts six to nine months but some go on for years as
some incompetent managers drag their heels - in some cases it is claimed
deliberately in the hope staff will quit their jobs.
During
this time suspended staff are banned from discussing the case or
contacting colleagues and some are even told they must not go to
hospital as a patient without permission.
The
annual cost of each suspension is estimated at £500,000 for doctors and
£50,000 for nurses, including pension costs, legal and admin costs and
hiring replacements.
The
disciplinary hearing of radiologist Dr Otto Chan, suspended in 2005
after he highlighted problems at the Royal London Hospital, cost £30,000
a day in lawyers' fees. The hearing began in June last year and went on
for six months.
We
also uncovered a number of appalling cases in some hospitals which some
NHS trust managers are desperate to keep under wraps.
In
the worst example we found, a highly qualified mental care nurse claims
she has been excluded for more than two years for raising concerns about
the safety of elderly patients. Another nurse has been suspended for
nearly six months after she complained of being sexually harassed by a
lesbian senior colleague.
Dr
Peter Tomlin, of the Suspended Doctors' Group of the Society of Clinical
Psychiatrists, said an average doctor is suspended for at least nine
months. He said: "Allegations about bullying are the easiest to
make and are very common indeed."
Our
investigation comes as the suspension of heart specialist Raj Mattu
drags into its fourth year. In 2002 he warned that "serious
overcrowding" in Walsgrave Hospital, Coventry was putting lives at
risk.He was ordered off the premises and legal action started to sack
him over claims of bullying.
While
there is no suggestion that the hospital trumped up the claims to keep
him quiet, he is now Britain's longest suspended doctor and his case has
cost taxpayers more than £2million.
We
sent Freedom of Information Act requests to all UK primary care trusts,
NHS trusts and care trusts asking how many doctors, nurses and
professionals are now suspended. Most have at least one. The numbers
could be much higher as staff are often put on "gardening
leave" - a way of forcing them to stay home without having to
register it as a suspension.
Some
trusts, such as Chesterfield and North Eastern Derbyshire PCTs,
University Hospital Birmingham and Homerton University Hospital, London,
used a clause in the Act to withhold information, claiming individuals
would be identified. Our figures for doctors are three times higher than
official government ones. The National Patient Safety Agency, which
records only numbers of suspended doctors in acute trusts, puts the
figure at 51.
While
there may be good reason for some suspensions, Barrie Brown, of nursing
union Amicus, claimed: "We believe there is a serious misuse of
suspensions and the Mirror's
investigation appears to confirm this. The key principle of suspensions
is to protect patients, not to deny them that protection."
Cause's
Julie Fagan claimed: "Very few suspensions are resolved quickly. It
goes into the pending tray and they get round to it when they can, so
staff can be left kicking their heels for months, even years.
"Some
investigations are often more like a witch hunt, a way of justifying the
suspension rather than establishing the truth. The person is rarely
allowed to give their side of the story. The distress this causes is
immense."
In
2003 the National Audit Office heavily criticised the NHS for
unnecessarily suspending doctors and nurses and allowing cases to drag
on for months, sending costs spiralling. But
even though the Department of Health issued guidelines urging trusts to
suspend staff only as a last resort, our findings suggest this is in
some cases being ignored.
Lib
Dem spokesman Steve Webb said: "Whistleblowers should be encouraged
to come forward, not penalised. In an increasingly commercial NHS,
making criticisms or raising questions is bad for business. "We
need a culture where professionals can speak freely without worrying
about losing their jobs."
Labour
MP Charlotte Atkins, a member of the Commons health committee, said:
"The Daily Mirror has shown suspensions are being used as a way of
muzzling staff."
The
Department of Health said: "These figures mean fewer than one
doctor or nurse in every 1,000 is suspended. But there is scope for
further reducing the number of unnecessary suspensions. "We
are tackling the suspensions culture head-on and have issued the NHS
with guidance encouraging employers to consider alternatives."
m.roper@mirror.co.uk
CASE
1
Anita,
45, a psychiatric nurse from Scotland on a £25,000 salary, has been
suspended on full pay for two years.
Two
years ago I raised concerns about the safety of elderly patients in my
unit. I had a quiet word with my superior because I believed it was in
the patients' best interests. He told me in no uncertain terms to keep
my mouth shut. I spoke to management who persuaded me to make a
complaint.
Days
later I was accused of bullying and harassment and sent home. I was
banned from hospital and it took more than six months to arrange a
meeting. They tried to transfer me, saying I needed to be re-educated in
working relationships. I refused.
Now,
over two years down the line, I'm still being paid my £25,000 salary to
stay at home. Patients' safety is
still being compromised but colleagues are too scared to speak. The
experience has devastated me.
CASE
2
Linda,
50, a district nurse for 20 years, has been excluded for six months from
a hospital ward in the south of England.
She earns £27,000. In my first two
weeks in a job at a city centre hospital, I was sexually harassed
by a lesbian senior sister. At first I kept quiet but it left me
traumatised.
Eventually
I complained but instead of supporting me, managers took seven months to
interview the nurse - then suspended me for six months. On a number of
occasions meetings have been arranged and cancelled at the last minute.
I believe they're trying to wear me down because they haven't got
evidence to sack me.
Being
suspended feels dreadful, humiliating and degrading, and I worry that
I'm losing the skills it took me years to learn. I had an unblemished
record as a nurse. All I ever wanted to do was to care for people, now
that's been taken away from me.
CASE
3
Auxiliary
Mary, 46, was sacked by her trust after being suspended for three
months. She was later cleared. She earned £20,000 a year.
I
WORKED as a nursing support worker for 17 years when I was suspended
without warning. I later found out
a member of staff had spread gossip about me stealing from the
department. The thefts continued after I had been excluded but
management wouldn't back down.
I
became depressed and went on medication. I was suspended for three
months before the trust fired me - without listening to my side of the
story. After four more months I was allowed to appeal. They rejected it
a month later but I was eventually cleared by tribunal.
My
happy nursing career was cut short because managers decided they wanted
rid of me, even if it meant ruining my life. The names and some details
have been changed to protect identities.
http://www.mirror.co.uk/news/paid-to-keep-quiet--name_page.html
BECOMING
A REGISTERED MENTAL NURSE
What is the work like?
Mental health nurses work in both hospital and
community settings to
support people with a range of mental health issues. They work
closely with clients and their families, friends and carers to develop
supportive, healing relationships.
As a mental health nurse, you would support people living with
conditions such as:
You could work with a variety of clients or specialise and work with
a particular group, such as adolescents or offenders. Your work could
involve:
-
counselling and support (either one-to-one or in groups)
-
using role play, art, drama and discussion as therapies
-
physical care, if the patient is too old or ill to look after
themselves
-
giving medication to patients.
You would work as part of a team including support workers,
psychiatrists, clinical psychologists and health visitors. You are also
likely to work closely with social workers, the police, relevant
charities, local government and housing officials.
What qualifications and experience will employers look for?
To qualify as a registered nurse you need to complete a Nursing and
Midwifery Council (NMC) approved degree or Diploma of Higher Education
in Nursing, specialising in the mental health branch.
To get onto an approved course you need to meet some general
requirements set by the NMC. These include:
-
providing evidence of your literacy and numeracy, good health and
good character, and recent successful study experience
-
meeting the minimum age requirement for nurse training – 17.5
years old in England
-
agreeing to have a CRB
check (a criminal conviction does not automatically exclude you
from working within the NHS).
For this branch you are likely to need previous experience, paid or
unpaid, of working with people who use mental health services. Course
providers can also set their own academic entry requirements, which can
include:
-
nursing diploma – five GCSEs (A-C) preferably in English, maths
and/or a science-based subject
-
nursing degree – usually the same GCSE grades as the diploma,
plus two or three A levels, possibly including a biological science.
If you do not meet the course entry requirements listed please check
with universities because alternatives such as an Access to Higher
Education course may also be accepted.
Some institutions offer an NMC approved Advanced Diploma in Nursing.
This qualification and the entry requirements for it lie between diploma
and degree level.

ABOUT THE NURSING &
MIDWIFERY COUNCIL
The Nursing & Midwifery Council (NMC) safeguards the health
and wellbeing of the public by continually regulating, reviewing and
promoting nursing and midwifery standards.
To achieve its aims, the NMC:
-
maintains a register of qualified nurses, midwives and specialist
community public health nurses
-
sets standards for conduct, performance and ethics
-
provides advice for nurses and midwives
-
considers allegations of misconduct, lack of competence or
unfitness to practise due to ill health
http://www.nmc-uk.org/aDefault.aspx
Fitness to Practise
The Fitness to Practise (FtP) Directorate processes allegations
of impairment of fitness to practise made against nurses, midwives and
specialist community public health nurses on grounds including
misconduct, lack of competence and ill health.
The overriding purpose of the proceedings is to protect the public
from unsafe registrants rather than punish them.
This section provides information on the work of the Directorate
including up-to-date Fitness to Practise (FtP) hearings and
decisions
http://www.nmc-uk.org/aSection.aspx?SectionID=7
WHAT
TO REPORT
Every
day employers, managers and supervisors of midwives deal with situations
concerning the misconduct, lack of competence or poor health of
registrants. Most of these incidents are managed at a local level and do
not give rise to wider concerns about public protection.
The
NMC’s role is to protect the public from registrants whose fitness to practise
is impaired and whose situation cannot be managed locally. In these
circumstances NMC committees can restrict or remove a practitioner’s
registration. Reporting a case of unfitness to practise to the NMC is
appropriate only when you believe the conduct, practice or health of a
registrant is impaired to the extent that public protection may be
compromised.
Fitness
to practise may be impaired by:
misconduct
lack
of competence
a
conviction or caution (including a finding of guilt by a court martial)
physical
or mental ill health
a
finding by any other health or social care regulator or licensing body
that a registrant’s fitness to practise is impaired
a
fraudulent or incorrect entry in the NMC’s register.
The
standards of conduct, performance and ethics expected of registrants are
set out in the NMC code of
professional conduct: Standards for conduct, performance and ethics (the
Code). While it is impossible to compile a definitive list of complaints
that the NMC investigates, the following examples will give you a broad
overview of situations that could form the basis of an allegation of
unfitness to practise.
Misconduct
Misconduct
is conduct which falls short of that which can reasonably be expected
of
a registrant.
The
most common examples of misconduct include:
Lack
of competence
Lack
of competence is a lack of knowledge, skill or judgement of such a nature
that the registrant is unfit to practise safely and effectively in any
field in which the registrant claims to be qualified, or seeks to practise.
Examples
of lack of competence include:
persistent
lack of ability in correctly and/or appropriately calculating,
administering and recording the administration or disposal of medicines
persistent lack of ability in properly identifying care needs and,
accordingly, planning and delivering appropriate care.
Conviction
or caution
The
types of conviction or caution that could lead to a finding of unfitness
to practise include:
theft
fraud
or other dishonest activities
violence
sexual
offences
accessing
or downloading child pornography or other illegal material from
the
internet
illegally
dealing or importing drugs.
Health
conditions
Health
conditions that might lead to a finding that a registrant’s fitness to practise
is impaired include:
alcohol
or drug dependence
untreated
serious mental illness.
How
to report a case to the NMC
All
allegations of impairment of fitness to practise must:
identify
the registrant concerned
clearly
set out the complaint against the registrant
be
supported by appropriate information and evidence.
A
check-list of the general information and evidence that is required to
support an allegation, as well as the specific reporting requirements for
the various categories of unfitness to practise, are detailed below.
All
allegations must include:
the
registrant’s full name, PIN and current or most recent address
the
registrant’s job at the time of the allegations and key aspects of the
post that may be relevant in considering the complaint
details
of any previous action undertaken through disciplinary, capability or
health procedures
Misconduct
Misconduct
allegations must include:
a
clear account of the alleged incident
a
brief description of the context or circumstances of the incident (for
example, the number and types of patients for whom the registrant was
responsible, and who else was on duty at the time)
copies
of witness statements and confirmation that the witnesses agree to give
a statement to the NMC’s solicitors and, if required, to give evidence
in person to a fitness to practise hearing committee
copies
of any relevant documents such as care plans and records, adverse
incident forms, medicine administration records, financial records and
work diaries
copies
of notes of any investigative or disciplinary meetings
details
of any police involvement and the name and contact details of the
officer in charge of the case.
Conviction
and caution
Cases
based on a conviction or caution must include:
the
name of the court, date of appearance and details of the offences
resulting in conviction
the
name and contact details of the officer in charge of the case (if
known).
Lack
of competence
Lack
of competence allegations must include:
details
of incidents which indicate a lack of competence (witness statements)
evidence
that the registrant has been informed about the deficiencies in their
practice (records of meetings and follow-up correspondence)
evidence
that the registrant has been given the opportunity to improve their
competence (objectives, action plans, appraisal records)
results
of assessments following opportunities for improvement that indicate a
continuing lack of competence (assessment records, witness statements).
We
strongly recommend you refer to the NMC booklet Reporting
lack of competence: A guide for employers and managers for
more advice about collecting evidence of lack of competence.
Health
issues
Allegations
about health issues must include:
a
clear account of any behaviour or incidents that show impairment due
to ill health
details
of the registrant’s sickness record and copies of any medical reports
confirmation
that witnesses agree to give a statement to the NMC’s solicitors and,
if required, to give evidence in person to a fitness to practise hearing
committee
copies
of notes of any meetings where the registrant’s health has been
discussed.
What
happens when you report a case?
Investigating
Committee
When
you send an allegation to the NMC, including all your supporting evidence,
we refer the case to a panel of the Investigating Committee. We also send
the registrant a copy of the allegations and supporting information and
invite them to submit a written response for the panel to consider. The
panel may ask for more information – for example, it can ask solicitors
to
carry
out further investigations or ask the registrant to undergo practice or
medical assessments. It can also invite you
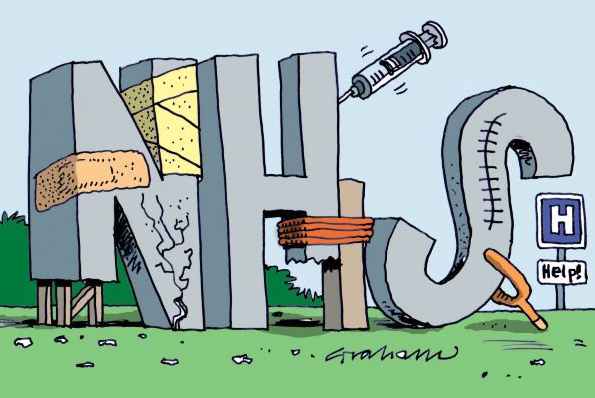
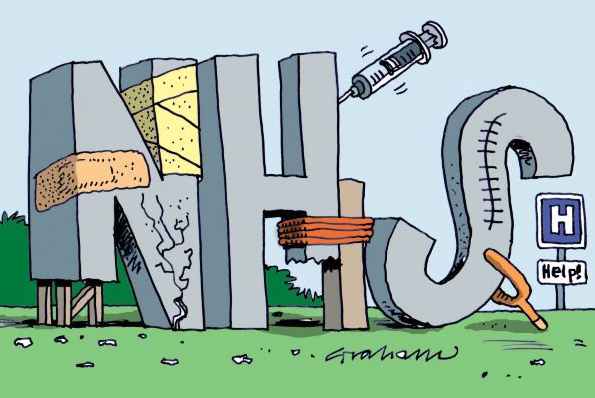
NHS
cartoon by Graham
SOME
PROMINENT MISCARRIAGES OF JUSTICE:
Simon
Hall
David
Watkins
Katie
Davis
Leon
Benjamin Forde
Warren
Blackwell
Darryl
Gee
Disclaimer
Some of the views expressed on this website are those of
individual contributors and do not necessarily represent the
views of SN. All content is for general information only and is
not intended to replace professional advice of any kind. SN is
not responsible or liable for any actions taken by a user of
this site. SN is not liable for the contents of any external
sites listed, nor does it endorse any advice, products or
services mentioned on these sites.
HUMANS:
|
SIMPLE
LIFE FORMS
|
As
in Amoeba, plankton (phyla: protozoa) |
|
ECHINODERMS |
As
in Starfish (phyla: Echinodermata) |
|
ANNELIDS |
As
in Earthworms (phyla: Annelida) |
|
MOLLUSKS |
Such
as octopus (phyla: Mollusca) |
|
ARTHROPODS |
Crabs,
spiders, insects (phyla: Arthropoda) |
|
CRUSTACEANS |
such
as crabs (subphyla: Crustacea) |
|
ARACHNIDS |
Spiders
(class: Arachnida) |
|
INSECTS |
Ants
(subphyla: Uniramia class:
Insecta) |
|
FISH
|
Sharks,
Tuna (group: Pisces) |
|
AMPHIBIANS |
Such
as frogs (class: Amphibia) |
|
REPTILES
|
As
in Crocodiles, Snakes (class: Reptilia) |
|
BIRDS
|
Such
as Eagles, Crow (class: Aves) |
|
DINOSAURS
|
Tyranosaurus
Rex, Brontosaurus (Extinct) |
|
MAMMALS
|
Warm
blooded animals (class: Mammalia) |
|
MARSUPIALS |
Such
as Kangaroos (order: Marsupialia) |
|
PRIMATES |
Gorillas,
Chimpanzees
(order: Primates) |
|
RODENTS |
such
as Rats, Mice (order: Rodentia) |
|
CETACEANS
|
such
as Whales
& Dolphins
( order:Cetacea) |
|
ANTHROPOLOGY |
Neanderthals,
Homo Erectus (Extinct) |
|
HUMANS
- MAN |
Homo
Sapiens THE
BRAIN |
|
LIFE
ON EARTH
|
Which
includes PLANTS
non- animal life |
|
|

New
energy drinks for performers
..
Thirst for Life
330ml
Earth can - the World in Your Hands
|
![]()
![]() logo and name Solar Navigator and Solar Cola are trademarks. All
rights reserved. All other trademarks are hereby acknowledged.
Max Energy Limited is
an educational charity.
logo and name Solar Navigator and Solar Cola are trademarks. All
rights reserved. All other trademarks are hereby acknowledged.
Max Energy Limited is
an educational charity.